
-
About Us
Discover more about CardioScan
-
Services
Our Service
-
Technology
-
Resources
Guides & Videos
Medical Resources
- Stroke
Chronologically, single chamber atrial pacing was first attempted at the dawn of cardiac pacing but was unsuccessful due to lack of hardware and programmability. Once overcome, it was now possible to implant atrial leads, but preference was given to dual chamber pacing systems. There are a number of ECG features which define single chamber atrial pacing but are poorly understood and will be discussed.
Single chamber atrial pacing can be identified on the ECG by a:

There are three programmed modes for single chamber atrial pacing.
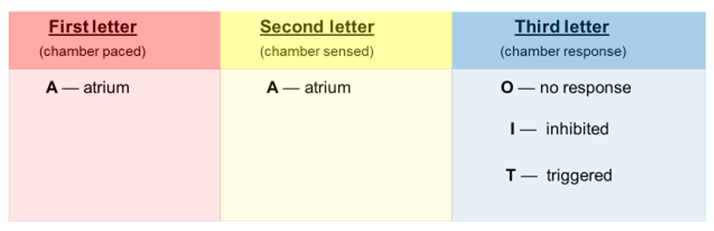
AOO Asynchronous
A Atrial pacing
O No atrial sensing
O No chamber response
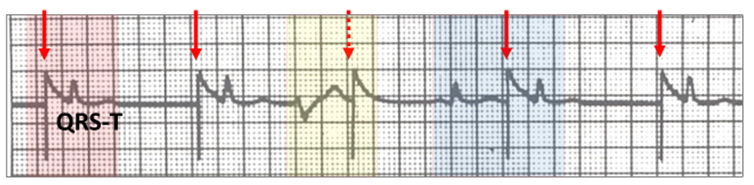
The unipolar stimulus artefact (red vertical arrow) continues unabated through the tracing. Provided the atrium is not refractory, there is a P wave hidden within the large stimulus artefact decay curve followed by a QRS-T wave (red highlight). In the presence of a ventricular ectopic (yellow highlight), the atrium is paced (red vertical stippled arrow) but does not conduct as the ventricle is refractory. When a sinus beat occurs it is not sensed (blue highlight), but if the next atrial stimulus artefact is outside the refractory period, pacing occurs with conduction to the ventricle.
AAI Atrial inhibited
A Atrial pacing
A Atrial sensing sensing
I Pacemaker output inhibited
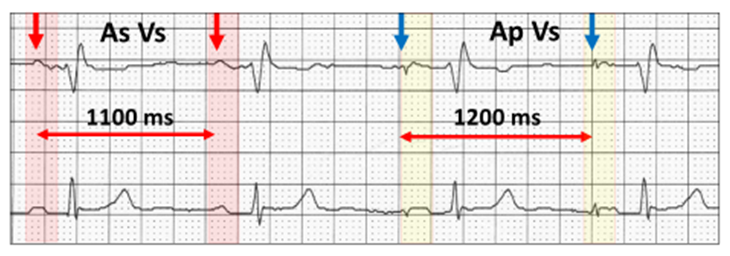
The stimulus artefact (blue vertical arrow) indicates atrial pacing (yellow highlight). When a sinus P wave occurs (red highlight), it is sensed, and the next paced beat is inhibited (red vertical arrow). The pacing cycle length is 1200 ms (50 bpm), whereas the sensed sinus cycle is faster at 1100 ms (55 bpm).
With single chamber atrial pacing, there is no recognition of native ventricular activity by the atrial channel unless it conducts retrograde to the atrium. Ventricular ectopics therefore, can be misinterpreted as pacemaker malfunction.
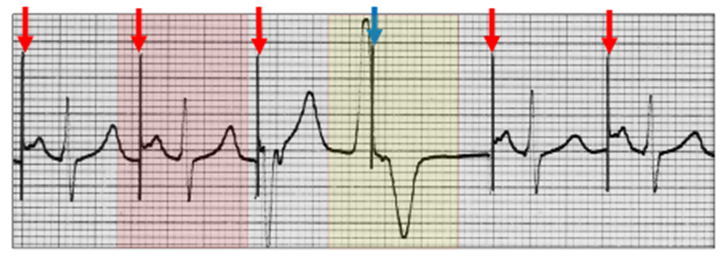
Unipolar atrial pacing (red vertical arrows) with normal AV conduction (red highlight). A ventricular ectopic (yellow highlight) does not interrupt the atrial pacing cycle (blue vertical arrow), but AV conduction is refractory. This is normal AAI pacing.
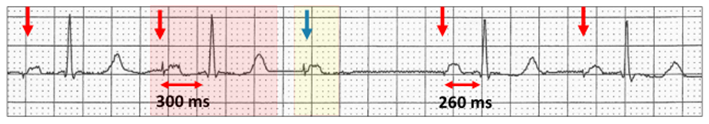
Ventricular ectopics occurring at the delivery of the atrial stimulus artefact may be interpreted as ventricular pacing. Both ECGs were reported as dual chamber pacing.
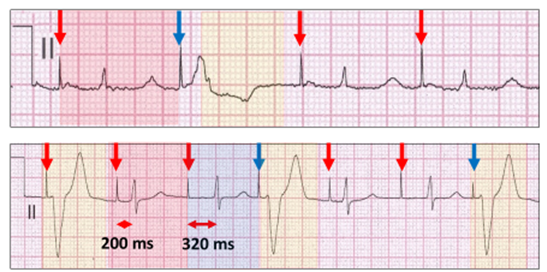
Above: Atrial pacing (red vertical arrow) with prolonged AV conduction (red highlight).
Below: Atrial pacing with Wenckebach AV sequences. The AV delay extends from 200 ms (red highlight) to 320 ms (blue highlight).
Because of the prolonged AV delay, ventricular ectopics appear late in the atrial pacing cycle soon after the stimulus artefact and simulate ventricular pacing.
How do we interpret this ECG?
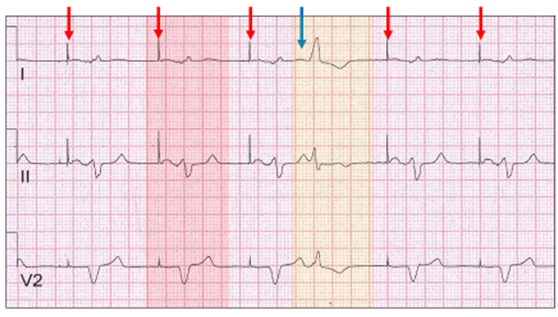
There is atrial pacing (red vertical arrow) and a broad QRS ectopic (yellow highlight). If this is single chamber atrial pacing, then the wide QRS is actually an atrial ectopic (blue vertical arrow) with aberrant conduction. The ectopic is sensed and explains the interruption in the atrial pacing cycle.
An alternate explanation is dual chamber pacing with ventricular sensing.
Atrial fusion beats may also occur but are rarely recognised.

The rhythm strip commences with an ectopic atrial rhythm (red highlight) which slows allowing atrial pacing (yellow highlight) to occur. Two atrial fusion beats intervene; first predominantly native P wave (blue highlight) and second predominantly pacing (green highlight).
When looking at the tracings with atrial pacing, it is important not to only focus on the pacing, as other abnormalities may be present.
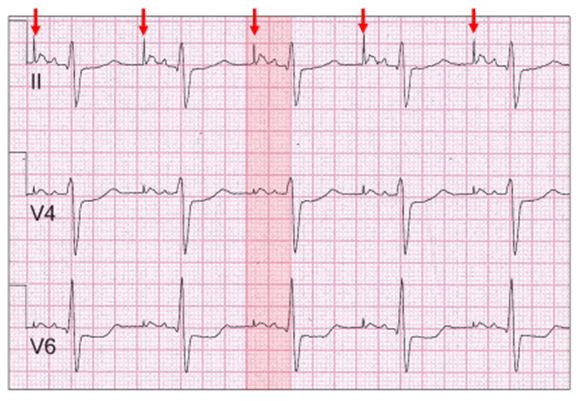
In this example, there is atrial pacing (red vertical arrow) and a marked left atrial abnormality with a broad bifid paced P wave (red highlight) characteristic of the pattern seen with severe mitral valve disease (P mitrale).
The AV delay is also very important in interpretation.
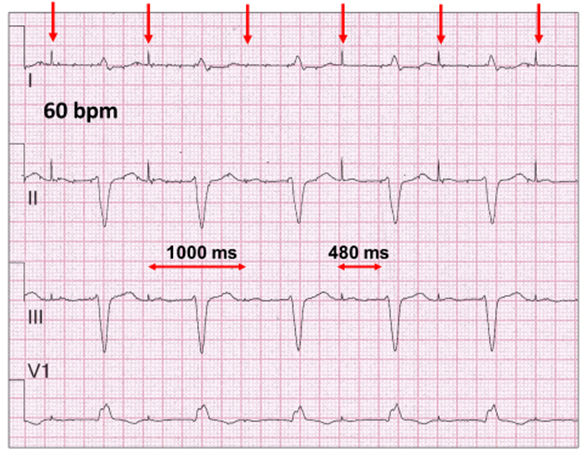
Atrial pacing 60 bpm (red vertical arrow) with a very long AV delay of 480 ms, which is almost 50% of total pacing cycle of 1000 ms (60 bpm). There is also a left anterior fascicular block and a right bundle branch block. Single chamber AAI pacing is inappropriate in patients with high degree AV block.
The prolonged AV delay is also important with pathophysiology. Even at a slow pacing rate of 60 bpm, the atrial stimulus artefact lies close to the T wave.
What happens when the atrial pacing rate increases with rate adaptive pacing?
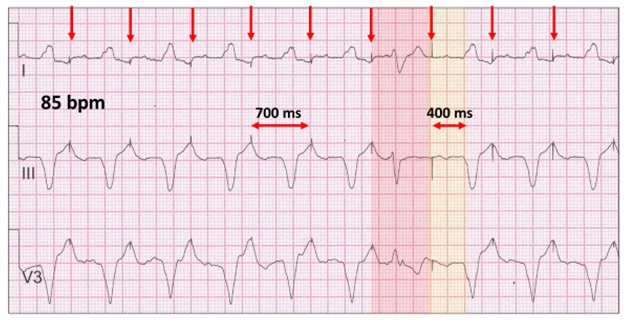
The atrial pacing rate in this ECG is 85 bpm. There is also a marked prolongation of the AV delay (400 ms) and a very broad native QRS suggestive of severe conduction tissue and ventricular disease. The atrial stimulus artefacts (red vertical arrow) lie at the peak of the previous T wave. Physiologically, the atria contract against closed AV valves equivalent to the pacemaker syndrome and clinically the patient describes this as “hitting a brick wall” on exertion.
This ECG also demonstrates severe atrial disease. There is a “premature” ventricular ectopic (red highlight) lying in the AV delay. The next atrial paced beat occurs beyond the T wave (yellow highlight). The P wave is either very broad or there is a latency period between the stimulus artefact and atrial contraction.
Wenckebach AV block is a common nocturnal finding in people of all ages
Therefore it may occur in patients with single channel atrial pacing and is not necessarily an indication to upgrade to dual chamber pacing.
AAT Atrial triggered
A Atrial pacing
A Atrial sensing
T Pacemaker output triggered
Atrial triggered pacing may be used in patients with single chamber atrial pacing when there is inappropriate sensing, particularly with unipolar leads.
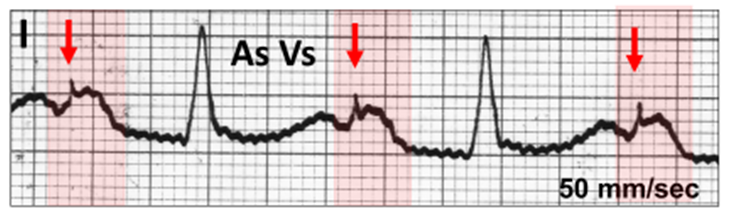
Following sensing of the sinus P wave, the triggered stimulus artefact (red vertical arrow) lies within the body of the P wave (red highlight).
Harry Mond.
In 49+ years as a practicing cardiologist, Assoc Prof Harry Mond has published 260+ published manuscripts & books. A co-founder of Cardiac Monitoring Service, he remains Medical Director and oversees 500K+ heart studies each year.
Download his full profile here.